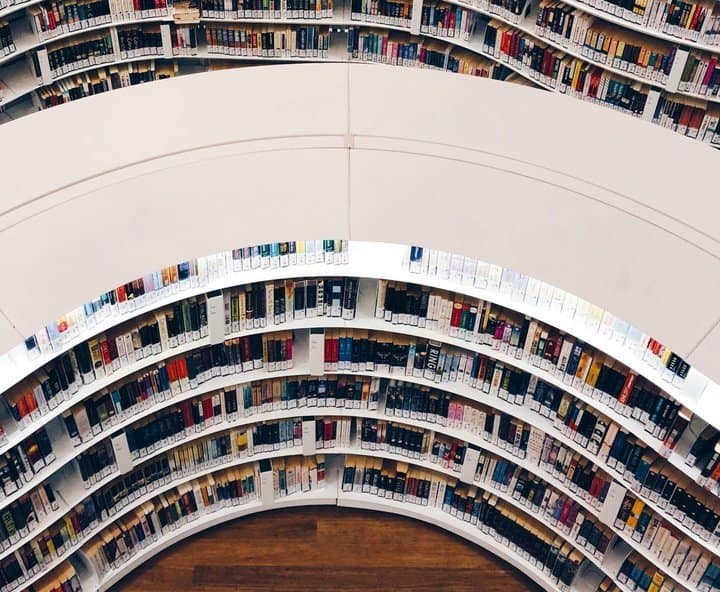
Embrace & Drive Change

Embrace & Drive Change
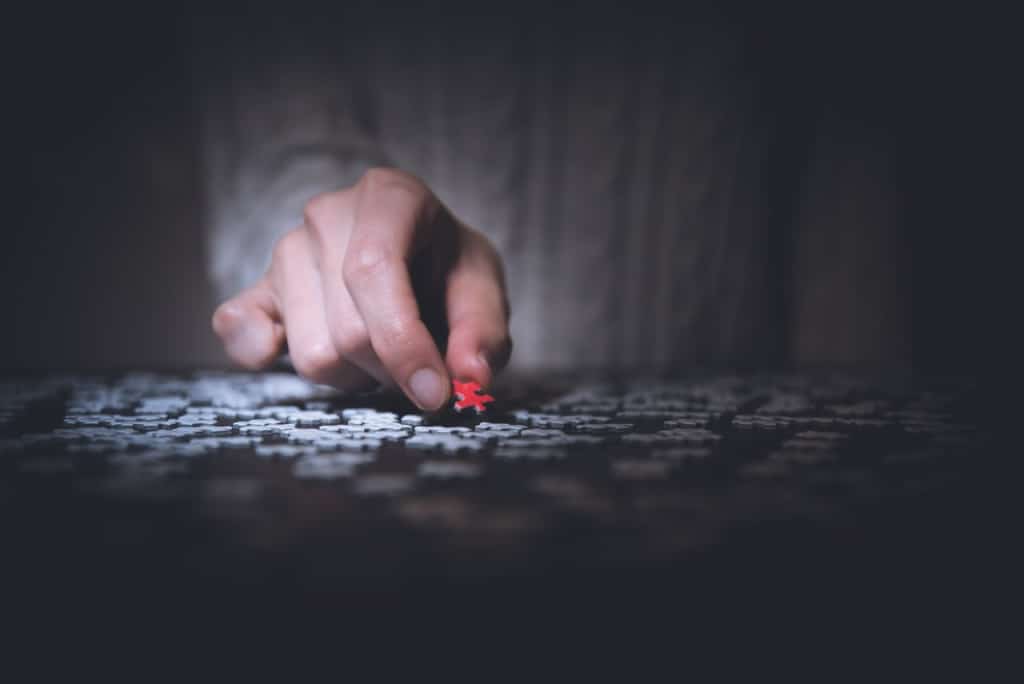
Our team are driving and inspiring innovative development into everything we do.
We encourage and support a culture of creativity and experimentation.
We continuously challenge the industry, and have been since 1996.